It might not seem like you’re doing a lot right now as you read this sentence, yet your eyes are tracking the words, your skin is generating an electrical current, your heart is beating, and it should be safe to assume that you’re breathing too. Let’s hope so.
This process occurs so instinctively that we don’t consciously think about them. Yet each can provide a new level of understanding of our behavior. Our respiration – a measure of breathing rate – is an often overlooked biosignal that can provide a deep understanding of emotional and physiological arousal.
Below, we will go through the mechanisms underlying respiration, how it can be measured, and what it can tell us about human behavior.
What is Respiration?
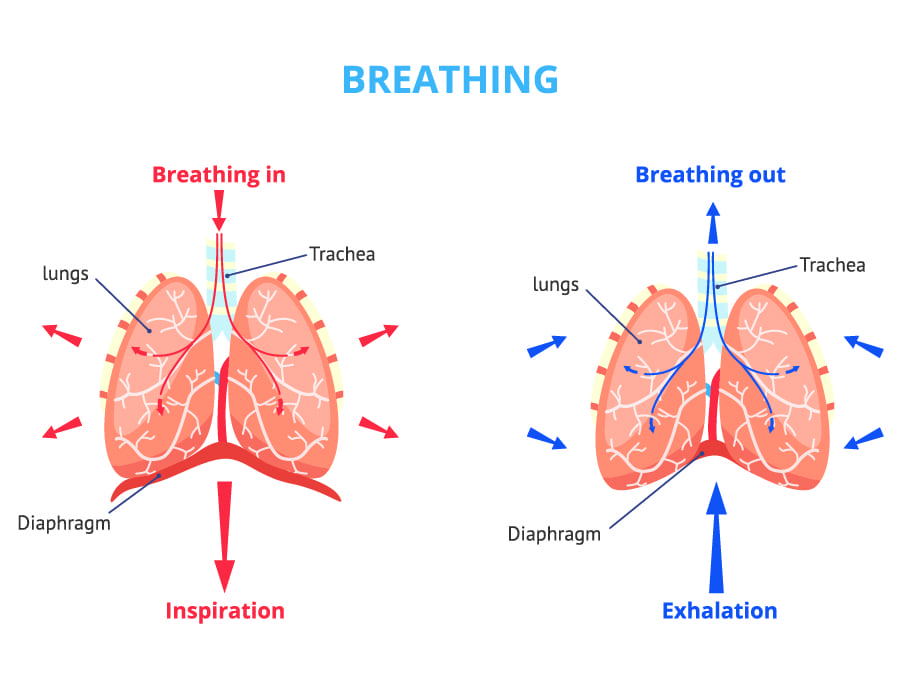
When we breathe, air is inhaled into the lungs, where oxygen is absorbed by our blood. This oxygen is essentially used to convert nutrients to energy (through the process of oxidation) that can be used by our cells.
At the same time that we breathe in, the lungs allow the carbon dioxide in our blood to diffuse outwards, which is then removed from the body as we breathe out. The whole process is known as respiration and is often recorded as respiratory rate.
Respiratory rate can generally be thought of as the number of breaths we take per minute. This is not the only way the data can be measured from a breathing individual – the variability of breaths over a set time period, and even the number of sighs can provide information about our cognitive, emotional, and physiological state.
Measuring Respiration Rate
In the past, respiratory rate was measured using manual approaches. When the participant or patient was at rest, the researcher or practitioner would count the number of breaths per minute.
Subsequent studies have found this approach to be somewhat lacking – a large margin of error has been found, with different individuals perceiving different numbers of breaths. Thankfully, a variety of devices are now available for measuring respiratory rate.
Respiration Devices
These devices measure the force of chest movements during respiration using a range of methods. Many require the use of a transducer belt and an amplifier.
The belt is worn by the participant and is sensitive to any changes in thoracic (between the neck and abdomen) or abdominal circumference. If using a belt ensure that it is fitted closely to the body. It also helps to have as little movement as possible while measuring the subject’s respiration rate, since too much movement can create noise in the data.

If you do observe noise in the data, it helps to differentiate whether this is physiological or due to movement by the participant. Using software with real-time capability can help with this. For example, if you observe an abnormality but simultaneously observe the participant turn in their seat, you know to ignore any strange data outputs.
Some devices will have different amplifier settings depending on research needs. It’s useful to have these different settings available so look out for them when selecting a product.
A physiological study looking at the effect of a particular exercise program, for example, will have vastly different requirements from a sedentary market research study. The amplifier stabilizes the signal received by the transducer and ensures it is clean and centered.
Normal Respiration Rates
To interpret respiration data, it is helpful to compare it to norms. For a resting adult, respiration rate varies from 12-20 breaths per minute. Under maximum exertion, the respiration rate typically hits 50 breaths per minute. In athletes the maximum respiration rate can reach 60 breaths per minute.
For children, the respiration rate is higher and continues decreasing till they reach 18 years of age. The steepest decline occurs in the first two years of life where the respiration rate decreases from a median of 44 breaths/minute to 26 breaths/min by the age of two. According to the CDC the following chart reflects a child’s respiration rate over the course of their development.
| Age | Respiratory rate (per minute) |
| 1 month | 40-60 |
| 6 months | 25-40 |
| 1-3 years | 22-30 |
| 4-6 years | 20-24 |
| 7-9 years | 18-24 |
| 10-13 years | 16-22 |
| 14-18 years | 14-22 |
| >18 years | 12-20 |
What Can Respiration Tell Us?
Variability in respiration rate has been shown to decrease during sustained attention – meaning that our breathing rate becomes more consistent when focusing on a task. This shows similarities to the behavioral correlates with heart rate variability (as these processes are essentially maintained by the same system, this is not too surprising).
An increase in respiration rate variability has also been associated with negative emotions, while the converse has been shown for fear responses. This shows one of the ways in which respiration can be related to emotional responses.
Respiration can also be used to provide information about the participants’ “sigh rate”. This measure is as you would think – data regarding the number of sighs. The process of sighing has been taken as a measure of resetting the regulation of both breathing and emotions – creating a sense of relief.
Together these measures have also been used to indicate the level of cognitive load a person is experiencing, data that can be critical in human factors domains.
Experimental design
Respiration sensors are versatile and can be used both within and outside of the laboratory. However, you still need to consider how your study design can influence your data.
Placement of the sensor
If you decide to purchase a respiration belt, then you will have to consider where to place it. A respiration belt is typically placed around the chest to monitor and measure a person’s chest movements during respiration. This type of belt can be used to monitor breathing rate and patterns, as well as to assess the effort and depth of breathing.
Alternatively, a respiration belt can be placed around the abdomen to monitor abdominal breathing, which is often used in certain clinical or research settings to assess breathing patterns or for biofeedback purposes.
The choice of whether to place the belt around the chest or the abdomen depends on the specific goals of the monitoring or measurement and the context in which it is being used. Both chest and abdominal belts have their applications, and the choice should be based on the specific needs of the situation.
Speaking during respiration recordings
In most cases, it is best to minimize speaking during respiration recordings to ensure accurate and consistent data. Speaking can introduce variability and artifacts into the recorded respiration patterns, making it more difficult to analyze and interpret the data. However, there may be situations where speaking is necessary or unavoidable during a respiration recording. In those cases, it is appropriate to have a way to recognize speech events, for example by recording the voice, and then exclude the respiration periods overlapping with speech, or, alternatively, analyze them separately.
Standing vs sitting
Collecting respiration signals in a sitting or standing position can lead to slightly different data due to the impact of posture on breathing mechanics. The postural change can also affect the placement of the sensor and thus the final data output.
Here are some key differences to consider when collecting respiration signals in these positions:
Diaphragm engagement: When sitting, people often engage their diaphragm more than when standing. This can affect the depth and pattern of breathing. In a standing position, the diaphragm may have to work slightly harder to support breathing.
Chest expansion: When sitting, the chest may expand differently compared to standing, which can affect chest wall movements during respiration. This variation in chest expansion can influence the respiration signal.
Postural changes: Standing and sitting involve different postural changes in the body, which can impact the alignment of the ribcage and diaphragm. These postural differences can affect how air moves in and out of the lungs.
Motion artifacts: Standing typically involves more body motion than sitting, so collecting respiration signals while standing may introduce more motion artifacts into the data, which can make the analysis more challenging.
Comfort and relaxation: Individuals may feel more comfortable and relaxed in one position over the other, which can affect their breathing patterns. This comfort factor can influence the respiration data collected.
In research or clinical settings, it’s essential to consider the specific goals of the respiration signal collection and choose the position that is most appropriate for the study or assessment. In some cases, researchers may collect data in both sitting and standing positions to account for these differences and obtain a more comprehensive understanding of an individual’s respiration patterns. The choice of position should align with the research question or clinical assessment being conducted, and the final decision should be preceded by pilot tests.
Conclusion
Incorporating the simple concept of breathing into your research can provide great insight into emotional and psychological processes. Stress and emotional arousal are both correlated with respiration rate, so investigating this factor can give you another angle – in terms of research, it’s a breath of fresh air.
Ready to use respiration in your research? Check out our respiration software module.
Free 29-page respiration Guide
For Beginners and Intermediates
- Learn about its anatomy and mechanisms
- Read about application in various research fields
- Overview of the different ways of collecting and processing respiration data